Breastfeeding Twins
Families and friends are always amazed when I mention that I am still breastfeeding my 2 year old twin boys. Having twins is a very different experience from having a singleton with respect to rearing and baby care but for me having twins has become a normal part of our family life. Once you overcome twin shock, you realize how lucky and blessed you are to not only have one baby but two. Unfortunately, although the incidence of twins is increasing due to fertility drugs and treatment, many mothers are discouraged from even attempting to nurse two babies. Mothers of twins need to know that breastfeeding their babies is realistic and possible, you can successfully nurse two babies for as long as the three people involved wish to do so.
Breastfeeding twins can sometimes be a challenge but the inherent rewards that come out of this experience usually more than compensate for any drawbacks. Mothers just need to seek out a little bit more help and organization at the beginning but once the wheel is rolling it becomes very hard to stop this great bonding relationship.
The health benefits of nursing twins are no different than for a single baby. Each baby receiving breast milk will have a reduced risk of developing asthma, food allergies and eczema; in addition s/he will be less likely to suffer from diarrhea, urinary tract, respiratory and ear infections. Breastfeeding may help in the development of the nervous system and contribute to increased intelligence quotient. Breastfed babies might also be at a lower the risk of childhood cancers, insulin dependent diabetes mellitus, and chronic bowel diseases. Breast milk is easily digested therefore resulting in less gas, colic and spitting up.1 Twins have a higher incidence of premature birth. Preemies benefit immensely from all the benefits of breast milk. Milk composition will change at each feed and as the baby gets older as well. Once the mature milk comes in, the composition of milk varies as well for mothers of twins. It is higher in fat, protein and immunoglobulin. No formula can compete with this golden milk that adapts and changes at each feed.
Of greatest importance, breastfeeding affords the baby closeness with its mother that bottle-feeding does not allow. Many mothers of twins find it difficult to bond with two babies at the same time but the great thing about nursing them, especially together, is that it allows you to really connect with the babies as four eyes stare at you or play in your hair. Mothers of multiple are also usually at greater risk of postpartum depression but it usually does not occur as readily in breastfeeding mothers. Some of my best memories are of my boys holding hands in the middle together while nursing or when one brother would stroke the other’s head. You never forget special moments like these.
The mother also benefits from nursing her twins because as the baby starts to suckle right after birth, the mother’s body releases the oxytocin hormone, which helps contract the uterus, decreasing postpartum bleeding. Since milk production burns about 500 to 1,000 calories a day, the nursing mother returns to her pre-pregnancy shape or weight faster than the non-nursing mother. Research shows that breastfeeding may reduce the risk of the mother developing breast, uterine and ovarian cancers.
One very important benefit is time saving. Being able to breastfeed twins together allows you to save time otherwise spent on bottle and formula preparation, sterilization of bottles and nipples. It allows you to quickly respond to the needs of two screaming babies and therefore reducing the amount of time during which the babies cry. It is estimated that mothers of twins will save on average 8-10 hours a week especially if the babies are nursed together as they do not have to spend this time on bottle preparation. Time is crucial when caring for two babies- you do not want to waste a single minute. Breastfeeding twins can also save you a lot of money! It has been estimated that you can save approximately 2000$ per year when you nurse twins. That money can definitely be used for other things around the house.
A lot of people do not realize that you can produce enough milk for two babies. It is important to remember that your body is very well designed and that the more often the babies are put to the breast the more milk you will produce. It is very rare that a mother will not be able to produce enough milk. Watch your babies’ signs, if they are wetting 6-8 diapers and soiling 3-4 diapers a day, then they are definitely getting enough milk. Remember that during their growth spurt babies can demand milk more often, these growth spurts usually occur at 7days, 3 weeks, 6 weeks, 3 months and 6 months. Babies also cluster feed in the evening and will be more demanding. If you can nurse both babies together you will secrete a higher level of hormones that will also help with your milk production. Make sure you are eating healthy snacks and food to compensate for the calories you are burning during nursing.
How do you hold two babies at once? Having a quality twin nursing pillow such as the E-Z 2 nurse by Double Blessings makes a huge difference in your level of comfort. I remember nursing both babies while simultaneously tying my older daughter’s shirt thanks to the E-Z 2 nurse. This pillow also allowed me to burp one baby while the other continued nursing. You can also try to stack some pillows around you as a makeshift platform. Experiment with different positions and holds and you will find one that works for you.
Here are some of the popular holds for mothers of twins:
- Criss-Cross cradle: in this position both babies are cradled in the crock of the mother’s arms. One body is behind the other forming an X
- Double football position: this is often a favorite position amongst mothers of twins. It does not usually put any pressure on the abdomen which will help if the mother has undergone a C-section. It also gives you a lot more control over the babies and there positioning.
- Cradle and Football: this is a great position for nursing toddlers together especially if one twin is bigger than the other. One baby is in the crock of the arm while the other one is in football position.

As a chiropractor I can not stress enough the importance of getting a baby’s spine checked for nervous interference from birth. Twins have a higher incidence of in-utero constraint as the space in the mothers belly is usually limited especially if the mother carries to term. If you are experiencing trouble nursing, it could be linked to subluxations in your child’s spine. A chiropractor, with the help of a lactation consultant, can help you identify if this is indeed causing a breastfeeding difficulty.
Nursing your twins can be one of the most rewarding experiences you will ever know. Mothers of multiples should seek help from a La Leche League group or a special twin support group. They can also contact a certified board lactation consultant who can help them prepare for the arrival of their babies. So next time you hear that someone is expecting twins, please encourage them to consider breastfeeding – it is the best gift of health for mother and baby that you can give.
Tips to successfully nurse twins or higher order multiples:
- Have an open mind
- During the first few weeks of adaptation get help with cooking and chores – you need to concentrate exclusively on the new babies and nursing
- Have confidence in your milk supply
- Avoid introducing artificial nipples and/or pacifiers to avoid nipple confusion which may interfere with obtaining a good latch
- Find a certified board lactation consultant who can help you
- Attend a support group such as La Leche League
- Read as much as you can on breastfeeding. The techniques are the same you just need to double everything.
- Find other mothers of multiples who have nursed their baby successfully
Dr. Valerie Lavigne
Chiropraticienne, DC
Motherhood and Back Pain
How many mothers and mothers-to-be do you know who complain of back pain? Quite a few, I’ll bet. As a new mother and a chiropractor, I can attest to the toll pregnancy and motherhood put on the back. A study in the journal Orthopedics reported that 50 to 90 per cent of pregnant women will likely experience lower back pain. Normally this pain diminishes after birth but it can persist, especially if preventive measures are not being taken.
There are two essential elements connected to the health of a spine: mobile vertebrae and a properly functioning nervous system. Vertebrae are responsible for the motion of the back, and problems occur when repetitive movements, poor posture, pregnancy, or trauma compromise this motion. Vertebrae also surround and protect the nervous system, so when an area of the back is not moving properly the nervous system is also jeopardized.
Back pain is caused by an accumulation of stress on the joints that can be triggered by an action as simple as picking up your child. As a reaction to the trigger, the body swells or becomes inflamed in that area, causing sharp pain. Back muscles also contribute to the pain by becoming tight or spastic in an effort to protect the spine. During pregnancy and afterwards, the body experiences many changes that can lead to back pain. Here’s why:
Pregnancy: There are three curves in our spine – in the neck, the mid-back and the lower back. The significant weight gain that occurs during pregnancy adds more pressure to the lower back and causes its curve to become more acute. The joints then have a greater potential to become inflamed and cause pain. The same applies to the neck and mid-back because of the increase in breast weight that pulls on the shoulder muscles. There is also an increase in the hormone relaxin, which causes ligaments to relax in preparation for the delivery. Its presence also creates abnormal motion in many joints, causing them to become inflamed.
Post-partum: Back pain can persist after birth. The loss of pregnancy weight once again causes a drastic change in the curve of the lower back. There is also the loss of the relaxin, which as it leaves the body tends to make ligaments tighter. This can cause the sacroiliac joint, the one used when bending forward to pick up a baby or get up from a chair, to not move as well as it should and create pain. Therefore, it is very important to verify that there is proper mobility in the pelvis area after delivery.
Infant and toddler years: Once the baby is born, there are countless mom-related daily activities, whether it is hoisting a car seat, wrestling with a stroller, carrying your toddler, vacuuming, or doing the laundry, that can cause your back to be strained.
Stiffness, usually in the morning, is the first symptom, and warning sign, that the pain may be a chronic problem. Don’t ignore it! As mothers constantly in motion, it is nearly impossible to not put some stress on our backs. There are ways, however, to prevent back pain and keep our backs working as optimally as possible.
Tips for a healthy back:
- Carry a backpack instead of an over-the-shoulder bag, especially if you are filling it with diapers, wipes, bottles, snacks, sippy cups, etc.
- When picking up your child, bend at the knees and bring your child close to your centre of gravity before lifting (this applies to lifting anything heavy). It is important not to hold the baby for prolonged periods on your hip because it will cause undue stress on the sacroiliac joints. It is much better to hold the child right against you with his legs wrapped around your waist equally.
- When reaching for something, make sure you don’t twist from your lower back – try to keep your feet pointing in the same direction as you reach. Twisting is one of the worst motions for the lower back as it does not tolerate it well and can cause serious damage to the disks between the vertebrae, like a discal hernia.
- Front pouches are not harmful as long as the baby is not too heavy and you do not feel discomfort or pain. Try to get a pouch that has a strap around the waist so some of the weight is distributed away form the shoulders.
- Exercise is important! An important component for both pre- and post-natal periods is strong abdominal muscles. They will support your lower back and lessen stress. You can start by doing a low number of crunches and slowly build up. Additional exercises are available from most chiropractic clinics.
Tips if injury or pain occurs:
- Apply ice for 10 minutes and remove for 20 minutes.
- Do not apply heat, as this will increase swelling.
- Try not to stay in one position for a long time – keep moving whenever possible.
- Sleep on your side with pillows between your knees or on your back with your knees up.
If the pain persists, you may want to consult a chiropractor. Chiropractic treatment is a manipulation of the spine to help ease the pain of musculoskeletal problems.
The chiropractor will perform an evaluation of the spine through a multi-component examination. There is a postural exam that allows the chiropractor to see if there are muscular imbalances and abnormal curves in the back and assess the gross range of motion in the lower back and neck to see how the joints are moving. The orthopedic exam narrows in on joints that are not working well. The neurologic tests verify motor strength and reflexes to see if the problem extends to the nervous system. Finally, the chiropractor will feel or palpate the motion of each joint of your back to find the problem area and verify muscle tension. She may also perform a radiological examination, to determine the degree of degeneration in the back, which will help with the prognosis and eliminate any risks during treatment.
The chiropractor will then work on the areas where there is a lack of motion and muscle tension by adjusting the vertebrae. The adjustment is not painful and creates that famous “crack” sound. The noise is caused by the accumulation of pressure in the liquid separating the two surfaces that make up the joints. By doing a quick move to open up the joint the liquid gets transformed into a gas and makes a pop. It is similar to the noise made by a can of soda opening and is definitely not the bones cracking.
The purpose of the adjustment is to restore motion, to reset the mechanism of the muscle spindles, which are needed for stretching and flexibility, and to trigger the secretion of endorphins, neurotransmitters in the brain with pain-relieving properties.
The chiropractor may also give you exercises to strengthen your back and keep it healthy.
No matter what, chronic back pain will simply not just go away. Even if the pain decreases, your motion will still not be as optimal as it was and the pain could easily be triggered again. Address the cause and you will feel much better.
Dr. Valerie Lavigne
Chiropraticienne, DC
Kids Need Chiropractic, Too!
A Child’s First Spinal Exam
- When is it time for a child ‘s first spinal examination?
- Should we wait until children complain of backache before taking them to the chiropractor?
These are two questions which parents frequently ask of their chiropractor. Throughout most communities it is a well-accepted fact that children should have regular dental check-ups to identify problems at the earliest possible time. In this way dentists attempt to identify early tooth decay and alignment problems of the teeth, because they know that the earlier the problem is detected the easier it will be to fix.
Well what about the potential for children to develop spinal problems? Should children be examined at regular intervals during their growing years to identify spinal problems which may progress to become serious, permanent problems. Unfortunately, the generally accepted view in most communities is that one visits a chiropractor for backache or neck pain, and in the absence of these symptoms, it can be assumed that the spine is doing okay.
When evaluating the spines of adult patients, chiropractors frequently encounter degenerative changes in discs and vertebral joint structures which have been ongoing for many years, without any evidence of symptoms. In many cases, it is only when the spinal degeneration reaches an advanced stage that symptoms of pain and stiffness occur. If the spinal problem causing these symptoms could have been detected at an early age, and the problem had been corrected, then a lifetime of misery due to chronic back pain could have been avoided.
Many of the worst spinal problems, which chiropractors detect on x-ray, show evidence of having been present for many years and can be identified, by the degree of degeneration, as having started during childhood. For this reason, it is recommended that a child’s first spinal evaluation should be early in life when the spine is growing and developing at the fastest rate. Orthopedists have identified that the time when the spine is most likely to develop problems, or for existing problems to worsen, is during periods of rapid growth.
Examination of the growth patterns of a child’s spine shows that the time of fastest spinal growth is during the first year of life, when the average length of the spine grows from 24 to 36cm. This is a 50 percent increase in one year, a rate which is unmatched in any other phase of a child’s growth and development. The next fastest growth rate occurs between the ages of one and five years when the spinal length increases from 36 to 51 cm, a 42 percent growth rate. Between the ages of 5 and 10, we see the slowest period of growth, 10 cm in five years, or a 20 percent growth rate.
The adolescent growth phase is most notable for its growth spurts, when a teenager may grow three to four inches in less than a year. The average total growth for the adolescent period is 20 cm in males and 15 cm in females, which represents a growth rate of 25 percent in females and 33 percent in males.
Now, taking all that into consideration, it can be seen that the period of fastest growth is the first year of life. The first year is also a period of considerable trauma when most children are learning to walk. This phase of a child’s development is also the period when the secondary spinal curves are forming in the child’s neck and low back. Because the first year of life is such an important one for spinal development, and because the potential for trauma is high, it is recommended that a child’s first spinal evaluations should be performed during this period. Beyond the first year, the child needs regular check-ups to ensure that the micro-trauma of a child’s daily living,
such as “rough-house” play and falls from bicycles, etc., are not causing spinal problems: problems which might otherwise go unnoticed simply because the child does not complain of symptoms.
Spinal growth and development continues right through until the mid-30s, when the development of the vertebrae in the lumbar spine is finally complete.
When we plant a tree in the garden, we stake and tie it to ensure that it grows straight during its early years. If we don’t do this, and the tree is allowed to bend with the wind for 10 to 15 years then it is impossible to straighten.
Don’t let your child’s spine develop like an unstaked tree. You don’t wait until your children complain of toothache before taking them to the dentist, so why wait until they complain of backache before having their spines checked.
Dr. Valerie Lavigne
Chiropraticienne, DC
Backpacks and Children’s Health
Originally published in ICPA Newsletter:
July August 2002.
For many students, “hitting the books” leads to academic achievement. Students who carry those books in overloaded backpacks may be unknowingly participating in the beginning of a health epidemic.
Scientific research reveals an alarming danger associated with improper childhood backpack use. This research stems from the increasing number of reports of childhood back pain in recent decades. By the end of their teen years, close to 60 percent of youths experience at least one low-back pain episode. And new research indicates that this may be due, at least in part, to the improper use of backpacks on young spines. That’s why Dr. Marvin Arnsdorff and his partner John Carroll created Backpack Safety America/InternationalTM to curb the rising tide of injury due to improper use of backpacks. “Back pain leads to more than 19 million doctor visits per year, according to the U.S. Department of Human Health and Services,” said Dr Arnsdorff. “What will that figure be when the members of the “Backpack Generation” are in their thirties and forties?” An increase in back pain appearing most frequently during the period of rapid growth — ages 11 to 16 is cause for concern.
BACKPACKS’ ATTACK ON BACKS
Watch children in any schoolyard struggle to walk while bent sideways under the weight of an overloaded backpack on one shoulder. You will quickly realize the potential danger of this commonplace item. How exactly does carrying a backpack affect the spine? Common sense tells us that a load, distributed improperly or unevenly, day after day, indeed causes stress to a growing spinal column. The old adage “As the twig bends, so grows the tree” comes to mind. There is a growing concern about the improper use of backpacks and the relatively scarce amount of instructional and preventative information available to young people. It is not the backpack’s fault that kids have not been given the guidelines.
CHECK THE NUMBERS
The Consumer Product Safety Commission estimates that 7,277 emergency room visits each year result from injuries related to book bags. The CPSC also reports that backpack-related injuries are up 330% since 1996. “That is the beginning of an epidemic, one that will cause serious damage to a child’s health for a lifetime,” said Dr. Arnsdorff.
GETTING OUT OF LINE
Hauling a heavy backpack over one shoulder everyday may cause serious postural misalignments. These postural imbalances often trigger a condition called vertebral subluxation. Vertebral subluxations are dysfunctional areas in the spine where movement is restricted or bones (vertebrae) are out of alignment. This disorder predisposes patients to a number of ailments, such as neck and back pain, headaches, and osteoarthritis.
In addition, a recent scientific experiment found that carrying a backpack alters the mobility of spinal bones and can lead to restricted movement-a risk factor for pain. Yet another study used magnetic resonance imaging (MRI) to examine the effect of backpacks on the intervertebral disc of the spine, the fluid-filled “pillows” between spinal bones. According to the report, backpacks alter the fluid content of these discs-a risk factor for disc herniation (“slipped” disc) and osteoarthritis.
BACKPACKS ARE NOT JUST CAUSING PROBLEMS IN THE UNITED STATES
The amount of weight carried by children in their backpacks is an important issue that deserves serious consideration. To quantify how much weight children are likely to carry in their backpacks, researchers in Milan, Italy, determined the weight of all the backpacks used by sixth graders at several schools.
The average load carried daily 20.5 pounds, reaching as much as 27.5 pounds, with the maximum daily load averaging 25.3 pounds. Over one-third of students carried more than 30% of their body weight at least once during the week.
A QUESTION OF BALANCE
Research presented at the American Academy of Physical Medicine and Rehabilitation’s annual meeting in San Francisco exposes yet another potential danger of heavy backpacks: they promote falls in students who wear them.
Specifically, students who carried packs weighing 25% of their body weight exhibited balance problems while performing normal activities such as climbing stairs or opening doors, which in turn increases their risk of falls. In contrast, students who carried packs weighing 15% of their body weight maintained their balance moderately well. Those carrying 5% of their body weight were most effective at maintaining balance, compared with their peers who carried more weight. In another recent study, children aged 10 to 13 stood on a platform that measured force. The children stepped from the platform onto a high step and back down to the platform.
The children did this three times — once without a book bag, once with the book bag carrying a load equaling 15 percent of the child’s body weight, and another time with a load equaling 20 percent of the child’s body weight.
The heavier the book bag, the greater the force children exerted to step up. There was also a trend toward greater impact forces when they stepped back down, the study found.
Dr. Mary Ellen Franklin, research supervisor commented, “Your body tries to keep the center of mass between the feet, so with a backpack, the trunk is in a more forward position, placing abnormal forces on the spine.”
“This requires shifting the head forward … but this would mean looking down. You compensate by bringing the head up, which makes part of the neck curve to a greater extent. It’s very stressful on the neck.”
ROLLER BAGS ARE NOT CURE-ALLS
An empty roller bag can weigh up to 80% more than an empty backpack. Factor in that there is a tendency to add more things to a roller bag, it can end up weighing 50 pounds or more. At some point during the day, a child needs to lift that bag, and proper guidelines still should be followed. Students, parents, and teachers are in need of specific safety guidelines necessary to prevent future spinal conditions due to improperly worn backpacks.
BACKPACK SAFETY TIPS
*Make sure the backpack is sturdy and appropriately sized. Some manufacturers offer special child-sized versions for children ages 5-10. These packs weigh less than a pound and have shorter back lengths and widths so they do not slip around on the back.
*Consider more than looks when choosing a backpack. An ill-fitting pack can cause back pain, muscle strain, or nerve impingement. You want to have padded shoulder straps to avoid pressure on the nerves around the armpits. Some backpacks have waist straps designed to stabilize the load. These should be used whenever possible.
*The proper maximum weight for loaded backpacks should not exceed 15% of the child’s body weight. For example, an 80-pound child should not carry more than 12 pounds in a pack. If the pack forces the carrier to bend forward, it is overloaded.
*In loading, it is obvious that excessive backpack weight can cause problems. Prioritizing the pack’s content is very important. Avoid loading unnecessary items. It is important to balance the weight of the contents or the body shifts into unnatural postures to compensate.
*Often ignored is the act of lifting and positioning the pack. Lifting 20 pounds improperly can cause damage.
Follow these simple steps:
- Choose a back pack with padded shoulder straps that fits your child’s size. ( A backpack that’s too large will sag towards the buttocks, stressing the child’s lower back and shoulders.)
- Lighten the load. Children should carry loads no heaver than 15 percent of their body weight.
- Face the backpack before you lift it.
- Bend at the knees.
- Using both hands, check the weight of the pack.
- Lift with your legs, not your back.
- Carefully put one shoulder strap on at a time. Never sling the pack onto one shoulder.
- Use both shoulder straps. Make them snug but not too tight. Carrying the backpack on one shoulder, while fashionable, can cause long-term neck, shoulder, back, and postural problems.
- Use the stabilizing waist strap around the waist.
- Look for signs — pain, red marks from straps, poor posture — indicating if a backpack fits poorly or is overloaded.
This article was contributed by the founders of Backpack Safety America/ International TM, the world’s first comprehensive education program designed to help students, parents and teachers prevent injuries related to the improper use of backpacks among school-age children. Doctors across North America and around the world have presented the program to more than a million students, parents, teachers and administrators. Their informative website offers practitioners, parents and children the opportunity to educate about the need for Backpack Safety measures. Visit them at: www.backpacksafe.com
Dr. Valerie Lavigne
Chiropraticienne, DC
The Benefits of Breastfeeding
Reprinted with the permission of Canadian Chiropractor magazine
In 2001, the World Health Organization (WHO) and UNICEF made the following recommendations for infant feeding: children should be exclusively breastfed for the first six months of life and thereafter should receive adequate and safe complementally food while breastfeeding continues for up to two years of age and beyond.(1) The Canadian Paediatric Society (CPS), Dieticians of Canada (DC), and Health Canada (HC) have endorsed these latest recommendations.(2)
As primary health-care practitioners, chiropractors are in position to discuss health and natural methods of healing by different means such as adjustments, nutrition and exercise. Every day in my clinic, pregnant patients ask for help to relieve the stresses of pregnancy. Some ask about the most natural, simplest way to feed a young child. Chiropractors who work in family practices should be knowledgeable in the basics of breastfeeding and be ready to direct patients to the appropriate resources.
Breastfeeding rates fell to an all-time low in the 1970s and ’80s in North America but things are slowly beginning to change as more people are realizing the benefits that breastfeeding brings to both the mother and child.
Breast milk is the ultimate food because it adapts and changes composition as a child ages, which infant formula cannot do.(3) Colostrum, which is the first liquid the mother’s breast secretes after childbirth, is very high in secretory immunoglobulin A, which helps the newborn fight off infections. Later, from the more mature milk, the baby still receives the same amount of secretory immunoglobulin A but it is diluted in proportion to the increased amount of milk consumed. The immunity transfer from the mother is crucial since children take up to five years to fully develop their immune system.
Breast milk is easily digested, therefore resulting in less gas, colic and spitting up.(4) Research shows that breastfed children may have a lower risk of developing asthma, food allergies and eczema,(5, 6, 7) in addition to less frequent diarrhea, and fewer urinary tract, respiratory and ear infections.(8,9,10,11) Breastfeeding may help in the develop- ment of the nervous system and contribute to increased intelligence quotient.(12,13) Breastfed babies might also have a lower risk of childhood cancers, insulin dependent diabetes mellitus, and chronic bowel diseases.(14, 15, 16,17,18) Of greatest importance, breastfeeding affords the baby a closeness with its mother that bottle-feeding does not allow. The breast- feeding child immediately after birth starts to use the senses of smell, taste, and touch.
Research published in Pediatrics in May 2004 claims that the overall mortality rate is 21% lower for breastfed babies compared to non-breastfed, and suggests that the longer babies breastfeed, the lower their risk of dying pre- maturely.(19)
As the baby starts to suckle right after birth, the mother’s body releases the hormone oxytocin, which helps contract the uterus, decreasing postpartum bleeding. Since milk produc- tion burns about 500 to 1,000 calories a day, the nursing mother returns to her pre-pregnancy shape or weight faster than the non-nursing mother.(20) Research shows that breastfeeding may reduce the risk of the mother developing breast, uterine and ovarian cancers.(21, 22, 23)
Nighttime feeding is convenient for the mother because there is no necessity to calculate and mix formula. Breast milk is always available and ready to use, making travelling with a young baby very easy. Nursing allows the mother to relax and rest during the day. It will require her to actually take the time to sit down and bond with her child. There’s an economic benefit, too, since breastfeeding can annually save a family as much as $1,500, the estimated cost of a year’s worth of formula.
Chiropractors in family practice might make available pamphlets that give information on breastfeeding and breast- feeding resources. A breastfeeding-friendly clinic would include a quiet area for moms to nurse, and could even provide supplies such as a feeding pillow, wipes, and even diapers.
La Leche League International (LLLI) was started in the United States in 1965 by seven mothers who wanted to help others learn about breastfeeding. The league offers phone support, monthly meetings and continuing education. In Quebec, a group called Nourri-Source also provides telephone support as well as weekly meetings at community centres where new mothers can come to weigh their babies and ask questions of the nurses who are present.
Women can also contact an international board-certified lactation consultant (IBCLC) whose role is to assist moms and provide them with evidence-based facts to help ensure breast- feeding success. These consultants undergo extensive breast- feeding education and a written examination, and they must re-certify every five years. They typically work in private practice, hospitals or clinical settings.
As the baby gets older, stronger, and more practised, breast- feeding becomes easier and faster with time. A new mother should be encouraged to continue with breastfeeding as long as it is satisfying for both her and the baby.
Assisting the next generation to get the healthiest possible start in life is a rewarding experience.
Dr. Valerie Lavigne
Chiropraticienne, DC
Breastfeeding Basics
This year’s theme for the World Breastfeeding Week is: Exclusive breastfeeding: the gold standard,safe, sound and sustainable. The World Health Organization currently recommends exclusive breastfeeding for six months and up to two years with other foods. 1So how can we help a new mother achieve this goal? Educating her on the basics of breastfeeding and helping her to fully understand how the relationship between mother and baby is formed should provide a step in the right direction towards a successful breastfeeding career.
New mothers often think breastfeeding is easy and natural, but if you’ve ever heard stories about difficult latches, thrush, mastitis, cracked nipples or any of the problems associated with breastfeeding, you know that it is really a learned art and sometimes a little help is needed during the learning process. As a new mother or a future new mother, you need to equip yourself with as much knowledge as possible to ensure that your breastfeeding experience is successful from the very beginning. This article will help you understand why “breast is best”, how to get a proper latch, and how to know when baby is getting enough milk.
By choosing to breastfeed, you are giving your child a huge advantage. The health benefits are immense, including a stronger immune system, fewer ear infections2, colds and upper respiratory infections3. Research has also shown a reduction in the incidence of diarrhea4 and asthma5 in breastfed babies, as well as IQ scores that are five to ten points higher than non-breastfed children6. The benefits to the mother are equally encouraging. We have seen a decreased risk of breast 7cancer and an easier recovery from delivery. Not to mention the huge financial savings breastfeeding can bring to the household — it has been estimated that a family of a singleton will save around $1,500 per year when baby is breastfed.
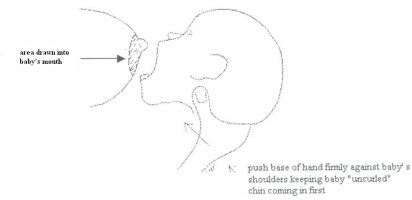
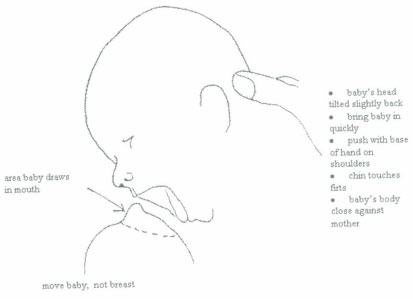
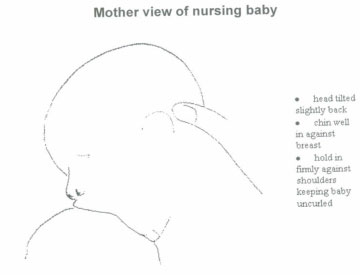
In his 1998 study, Righard estimated that 94% of mothers experiencing breastfeeding problems had incorrect positioning and latch-on8. The single most important breastfeeding skill to understand is how to put a baby to the breast efficiently. This is called latching the baby. When a baby is well latched, she is massaging the milk ducts and thus able to extract milk. If the baby is not positioned properly on the breast, she will not be able to create the stimulation necessary to empty the milk ducts and therefore produce more milk. Remember, it is baby who regulates how much milk is made, not mom! Simply put, the more often the breast is emptied, the more milk will be produced. Understanding this basic skill is the first step toward successful breastfeeding.
Latching on:
To latch your baby effectively, you should be seated comfortably in a chair or on a couch. Once the general concept of latching is understood, you can then breastfeed in various positions. Your back should be well supported and reasonably straight; your feet should also be well supported on the floor or on a footstool. This is supposed to be a fun experience so try to relax as much as possible!
It is important to understand that latching means it is the baby who is going to the breast, not the mother putting the breast into the baby’s mouth. When baby comes into contact with your chest she will move into an instinctive position. This is described by Glover (2000) as the baby tilting her head back and leading with her jaw and mouth to the breast9; her mouth is wide open, tongue down and over the bottom gum line to take the breast. This results in the baby having a large amount of areola/breast tissue in her mouth. Her chin should be firmly pressed against the breast and she should be able to breath freely through her nose. Remember that it is BREASTFEEDING NOT NIPPLE FEEDING – the baby needs to have this large amount of the breast in her mouth to be able to stimulate the milk ducts.
How can you help your baby with this process? Let’s look at the cross cradle position with baby on the right breast. First, you will hold your baby’s neck between your left thumb and index underneath the ear with a solid grip. The baby will be chest to chest with you and you will be supporting her back and shoulder with your left arm straight. With your right hand, gently squeeze your breast in a “C” or “U” shape, making a kind of “hamburger” to facilitate the latch. The nipple should be pointing towards the top lip. Then the game of patience begins — you will need to wait for baby to open her mouth WIDE. When this occurs you will quickly pull her towards you and place her on the breast, rolling the nipple under the top lip. Both lips should be flanged out.
You should then see baby starting a sucking pattern with small sucks that stimulate the milk to come down. After let-down, the sucking should look like open-pause sucks: the baby will pause mid-suck, her chin dropping down a fraction — she is now transferring milk and swallowing. It is important to be able to recognize the difference between sucking and swallowing.
To facilitate latching, you should put your newborn to the breast as soon as possible after birth. This is easily accomplished if mother and baby room-in together. There should be no time restriction placed on nursing – put away your watch and let yourself be guided by baby’s cues. The early cues include rooting (when you stroke her cheek and mouth, baby will turn her head to seek the breast with an open mouth), placing her fists in her mouth or making sucking motions in her sleep. The breast should be offered as soon as baby exhibits any of these signs of hunger. As long as your baby is sucking in an open-pause-close rhythm, she should remain on the breast. Crying is a late cue, so by this time the baby is VERY hungry and latching can be a little more difficult. To help baby get more milk and keep her actively sucking on the breast, you can do breast compressions: you will hold the breast, compressing it for 5 seconds and then releasing. Usually within a few compressions, baby will start another rhythmical sucking pattern. Remember, it is not normal to have pain! If pain occurs the baby is not well positioned and this could result in damaged nipples. In addition, no artificial nipple should be introduced in the first six weeks.
When do you know if baby is getting enough milk? First, you need to recognize the open-pause sucking rhythm. This tells you that baby is transferring milk and swallowing. Secondly, what goes in must come out — baby should be producing about six to eight wet diapers daily and having three to five bowels movements.
It is also important to recognize when your baby is going through growth spurt. Baby will change her feeding pattern and probably start nursing significantly more often. This is your baby’s way of telling your body that she needs more milk. Growth spurts usually occur at around three weeks, six weeks, three months and six months old. Your baby’s feeding pattern will eventually go back to normal after these periods of what feels like non-stop nursing.
Throughout your baby’s development and growth there are key times it is essential to bring your baby in for a spinal evaluation. Right after birth is so important because of the potential traumas to the spine and cranium from birth. Any difficulty you may be having breastfeeding your little one may be caused by misalignment of the spinal or cranial bones. These would include difficulty in latching on, what seems to be discomfort when the baby nurses or a baby favoring one breast or the other. By evaluating your baby’s neck, musculature and nervous system, your doctor of chiropractic can ensure that the sucking mechanism is functioning well therefore allowing the baby to open as wide as possible. Your doctor of chiropractic will also help in situations when a baby refuses to suck or clamps down too fast on the mother and is not maintaining a big open mouth. Your doctor of chiropractic will perform a spinal evaluation to detect any subluxations and will also concentrate on the jaw area because of its involvement in the sucking mechanism. A craniosacral evaluation can also help detect any problems around the cranium that may have resulted from the delivery process and could have an impact on breastfeeding.
If problems do occur, contact a certified lactation consultant and your doctor of chiropractic for help. These two professional will be able to assess what is causing the problem. You can also contact your local La Leche League group for advice and mother to mother support. If you do not yet have a Family Chiropractor, check out this website for one near you: www.icpa4kids.org . Do not wait! The faster your problems are addressed, the faster they are solved.
Breastfeeding is one of the best things you can do for your baby so enjoy every minute of it. They really do grow up fast! Don’t be shy to get some help to ensure a proper start and continued success in this wonderful experience you will share with your baby.
Reprinted with the permission of Pathways Magazine: www.icpa4kids.org
Dr. Valerie Lavigne
Chiropraticienne, DC
Weight limit recommendation in backpack use for school-aged children
Lavigne V. Weight limit recommendation in backpack use for school-aged children, J Clin Chiropr Pediat. 2014, Vol 14-2, March 2014
view the whole article here (pdf)
Background:
Every day children use backpacks to get their books back and forth from school. Many children carry very heavy backpacks and there are some concerns that this could be contributing to back pain in children. Objec- tive: The purpose of this paper is to assess, using the literature, what is the recommended weight limit that should be carried by school-aged children. Discussion: Many organizations, such as Back Pack Safety International, are trying to educate children on how to wear their backpacks properly and on the weight limit those children should carry to minimize back pain. However, many factors such as design, weight, how it is worn, and children’s physical fitness have been shown to have an influence on the development of pain caused by backpacks. As well, parents and teach- ers have a determining role in helping children be better organized to have lighter backpacks. The literature does not seem to agree on a set weight limit but it is shown that to prevent back pain it should definitely not exceed 10-15%. Conclusion: Backpacks have an influence on back pain in children and the weight limit should not exceed 10-15% of the child’s body weight.
Introduction:
Children around the world use backpacks to carry their school supplies to and from school. Studies show that at least 90% of school children in the developed world are us- ing backpacks every day1,2. The weight of backpacks carried by children is creating growing concerns amongst school administrators, parents and healthcare professionals3. Ne- grini and Carabalona (2002) reported that the average daily load of Italian students over a week ranged from 22% body weight (BW) to 27.5% BW with some students wearing backpacks weighing as much as 46% of their BW, exceed- ing the 30% bodyweight/load ratio proposed for physically fit adults4,5. Some researchers hypothesize that heavy back- packs may be contributing to back pain in school-aged chil- dren2,6.
A child’s constantly developing spine experiences the high- est rate of growth between the ages of 10-12 for girls and 13-15 for boys, with the secondary centers of ossification not fusing completely until the mid-twenties. At this stage, when the spine may be more susceptible to injury, proper backpack use is crucial to preventing postural deformi- ties7,8. As well, it is shown that by adding weight to the back with a backpack, the center of gravity is shifted forward to- ward the rear of the base of support. Postural compensa- tions are needed to maintain balance and functional motion during gait; however, with improper loading of backpacks these postural compensations can result in injuries to the child’s spine. Some of these compensations include an in- creased forward head carriage, an increase in forward lean of the trunk, as well as changes of pelvic positions and gait patterns. Grimmer et al. (2002) found that more than 20%
of students in each age group had a mean change of 5° in craniovertebral angle (CVA) with the greatest changes in the smaller age group9,10. The degree of posture change in these children is comparable to the change in CVA in adult women suffering from headaches4.
To try to prevent back pain caused by backpacks, safety tips and information on choosing the right backpack, on how to fill it properly and how to wear it correctly, are available from various websites including the American Academy of Pediatrics11, The American Academy of Orthopedics12, Back Pack Safety International13, American Chiropractic Associa- tion14, and numerous other sites for parents, teachers and school-age kids4,15. Different methods of wearing backpacks have been recorded, for example, some studies showed that 73.2% of students carried with one shoulder. This carrying method seems to be decreasing in the United States with the help of backpack education programs that emphasize even weight distribution to avoid torqueing the spine4.
Back pain in school-age children is becoming a common complaint, with a prevalence ranging from 30%-65%2, 6, 16. Unfortunately, some evidence in the literature shows that children suffering from low back pain may still have pain into adulthood; therefore, prevention is becoming impor- tant17-19. A factor contributing to this high prevalence of back pain in children stems from their increasingly seden- tary lifestyle, with more time spent in front of the computer or television. As well, there are some thoughts that the load- ing of the spine with backpacks every day is contributing to the issue2, 5. It is believed that a certain amount of stress or load on the spine may contribute to its strength, however, excessive and repetitive stress on a child’s body may result in overuse injuries. Some injuries reported with backpack use are low back pain, neck pain, shoulder pain, muscle soreness, and rucksack palsy2. Other problems associated with backpack use have been reported including respira- tory problems, winged scapula, foot blisters, tripping ac- cidents, and getting hit by the backpack20, 21. Siambanes et al (2004) surveyed 3,498 Southern California adolescents and found that 41.3% reported pain when carrying backpacks, with 16.9% consulting a doctor for the pain and 16.1% re- porting missing school activity due to pain22. Korovessis et al. (2004) studied a sample of 3,141 Greek students be- tween 9 and 15 years old that showed an increase in dorsal pain correlated to increased backpack weight23. It has also been reported that girls usually experience more pain with backpack use than boys4, 15, 24, 25. It is important to note that these complications have not only been associated with the school bag load, but also with the duration that the school bag is carried. Increased duration will cause fatigue and pain; therefore, limiting only backpack weight may not be the solution5. The literature is unclear regarding the recom- mended weight for children — there is some debate whether the cutoff should be no more than 10% of the BW or up to 15% of the BW.
This paper will review the literature to assess what is the recommended limit for backpack weight worn by school- age children.
Methods:
The search was performed using PubMed with the follow- ing terms “backpacks and children” with limits of “review” and language “English”. This resulted in eight papers, which were all kept for analysis. A second search using the terms with no limits “backpacks and children” revealed 60 articles – 14 were kept for references. The articles not kept did not discuss backpack weight limits specifically and were not re- tained. The articles were hand-searched and 3 more articles were retained. Evidence-based medicine (EBM) has a hier- archy that puts systematic reviews at the top of a pyramid followed by randomized control trials, cohort studies, case- control studies, case series, case reports and editorials and opinions26, 27. The results of this search will be explained in order of highest evidence available according to EBM.
Results:
Lindstrom-Hazel (2009) produced a systematic review of the literature looking to answer three questions. First, she asked, “Are school-age children at risk for back pain because of carrying backpacks? How much load is too much?” Secondly, “Does backpack in adolescence predict back pain in adulthood? and thirdly “Are there behaviors that lessen/increase the risk of back pain/injury?”15. The
review was well performed with explained search meth- ods and tables showing the relevant articles. The conclu- sions were that girls are more likely to experience back pain than boys, that the time carrying a pack may be a strong contributor to pain, and psychosomatic behavior may con- tribute to back pain. Lindstrom-Hazel (2009) reported that some authors were strongly calling for a weight limit; how- ever, she believed that, up to this point, scientific studies had not yet produced consistent results that allowed her to wholeheartedly endorse safe limits that would protect all children. She believed that the issue of back pain was mul- tifactorial including weight, time carried, and child’s height in relation to the backpack. She concluded that back pain in children was a strong predictor of back pain in adult- hood. She also reported that, although many organizations have various recommendations for backpacks, many stu- dents still choose their pack according to color and size. It can be assumed that many students do not understand the risk of back pain later in life; however, programs are in place to educate parents and teachers on avoiding unneces- sary backpack weight. Therefore, according to this review, weight recommendations are not consistently supported to prevent back pain in children.
Brackley et Stevenson (2004) produced another systematic review trying to determine whether the suggested weight limit of 10-15% BW by certain organizations was the appro- priate limit for school-age children and supported by the literature2. Their approach to the question was interesting because they separated the literature according to three dif- ferent effects of backpacks use. They looked at the various literatures discussing the physiological consequences, the biomechanical consequences, and backpack design for chil- dren. By looking at the effects of backpack use in differ- ent ways, this review was the most complete. The search method was well explained and it included tables summa- rizing the research articles. The conclusion based on the lit- erature, combining the three effects of backpack use, was that 10-15% BW is a justified weight limit. Further research is required to determine the association between backpacks and injury, and the way in which load, backpack design, as well as personal characteristics such as physical fitness, interact and influence adaptations required when carrying a backpack.
Kistner et al. (2012) looked at a small cohort study of 11 school children aged 8-11 years to examine the various ef- fects of backpack loads on posture and postural compen- sations by evaluating forward head carriage4. The results showed immediate and statistically significant change in CVA, indicating increased forward head positions when us- ing backpacks containing 15% and 20% BW. When students carried backpacks with 15% and 20% BW, more than 50% of the subjects reported discomfort after walking, with the neck as the primary location of reported pain. The conclu- sion was that backpack loads should not exceed 10% BW due to the increased forward head position. One limitation to note from this study is the small sample size.
Rodriguez-Oviedo et al. (2012) produced a cross-sectional study in Spain that investigated whether backpack weight is associated with back pain and back pathology in school children25. Their results showed that 61.4% of participants carried backpacks exceeding 10% BW and 18.1% exceeded 15% BW. The children carrying the heaviest backpacks had a 50% higher risk of back pain and a 42% higher risk of pa- thology with girls showing a higher risk of back pain than boys. They encouraged the medical community to advise parents and school children about the risks posed by heavy school bags and the fact that this risk can be easily reduced.
Moore et al. (2007) produced a cohort study looking at 531 students in 5 different California schools from 5th to 12th grade and their backpack weights. This study weighed the backpacks and students were then individually inter- viewed about how often they experienced pain while car- rying a backpack, the site of their pain, and if it interfered with activities. The data supported the use of a 10% BW cutoff for safe backpack use for all grade levels and that girls were more at risk for back problems.
Discussion:
When analyzing the literature regarding backpacks, it is challenging to recommend a weight limit that would pre- vent injury in all the children due to the multiple factors involved in the development of pain, i.e. design, weight, how it is worn, and children’s physical fitness. Negrini et al. (2002) suggested time worn was also important to con- sider when analyzing the effects of backpacks5. Macias et al. (2008) concluded that perceived pain in the low back was significantly higher while wearing the backpack on one shoulder versus two shoulders1. If one looks at the evi- dence, the systematic reviews (considered higher evidence in evidenced-based medicine) had conflicting conclusions and therefore were unable to suggest a clear weight limit. These reviews agree that more research is needed. Smaller studies performed more recently point to a 10% BW but they are generally focusing on only one factor, such as bio- mechanical changes. There has been no research performed to date that considers all factors in their evaluation and analysis. It would be worth doing other studies, with more subjects, and analyzing many factors simultaneously to see if the 10% cut-off point should be recommended.
As chiropractors, it is important to incorporate questions regarding backpack use when taking the history of a child. This information can help point the chiropractor towards some of the possible causes of back pain and should open
up the discussion with the child and parent on how to carry books and appropriate weight limit. The chiropractors can then incorporate these recommendations when preparing the treatment plan of the child.
Many people, including chiropractors, have a determining role in trying to reduce the weight children carry in their backpacks. Parents should be sensitized to the weight of the backpack as well as the distance the child has to walk to and from school, as well as the design and wearing technique of the backpack. Teachers can influence the children when it comes to what material needs to be brought home daily. They should be sensitized to the changes of posture created by poor backpack use so they understand the importance of proper use. When they are planning their weekly cur- riculum, they could do so according to the textbooks chil- dren will need on a specific day and assess what goes in the children’s backpacks5. As part of the weekly routine, teach- ers could have a scale to weigh backpacks and encourage students to lighten their load. Also, to emphasize physical fitness along with a properly fitted backpack, physical edu- cation classes could include relay races while carrying the backpack.
In this era of technology, they can make use of e-books and reduce the number of textbooks needed with the use of smart tablets like the iPad. A word of caution is needed here — the use of computers by some schools has actually increased the load students’ carry because a specially designed backpack, which is already heavier, is required. Before switching to digital textbooks, we need to ensure that technology does not, in fact, increase backpack weight. Students need to learn how to make good choices when loading their packs, including choosing to carry only things that are absolutely necessary and not everything they think they might need or want to bring home. Furthermore, they should be taught to load bigger books in the back so to decrease stress on the shoulders. Parents should also make sure that the backpack contains no loose or dangling cords, strings and piece of clothing. These can catch while the child is walking, make them fall and create an injury that could be tragic if it got caught in the door of the bus28. With support from parents, the school curriculum should include a component of total backpack use including loading, lifting, holding, wearing, organizing, clearing and storing at school, to help prevent back pain in children.
Conclusion:
It is evident that backpacks have an influence on back pain in children, but it is not clear if this pain is caused by weight alone or by multiple factors such as design, time worn, and physical fitness of the child. It seems difficult to design a backpack that would be suitable for all children and us- able in every situation. It is fair to say that backpack weight should not exceed 10-15% BW, however the backpack weight appropriate for each child should be determined individually.
Dr. Valerie Lavigne
Chiropraticienne, DC
Breastfeeding and Dental Caries
Lavigne V. Breastfeeding and Dental Caries: Looking at the Evidence Clinical Lactation 2013, Vol.4-1 Page(s): 12-16
view the whole article here (pdf)
Dental caries and prolonged breastfeeding still trigger much debate among professionals and parents. Some mothers are still being told to discontinue breastfeeding their toddlers because of cavities in the mouth. Parents often feel very discouraged and upset when they are forced to stop breastfeeding their toddlers. Dental caries is one of the most common chronic diseases in childhood, and is a disease of multifactorial etiology. This paper reviews the literature on dental caries and breastfeeding. This review revealed that there was no conclusive evidence that prolonged breastfeeding increased the risk of early childhood cavities.
Mothers around the globe are encouraged to breastfeed according to the recommendations of the World Health Organization, which states that babies should be exclusively breastfed for the first six months, and up to two years and beyond with the addition of complementary food (World Health Organization, 2011). The Canadian Pediatric Society also endorses these recommendations. The health benefits of breastfeeding have been shown to reduce sudden infant death syndrome, otitis media, asthma, breast cancer, and accelerate postpartum weight loss. However, the American Academy of Pediatric Dentistry (AAPD) does not endorse the recommendation of extended breastfeeding past 12 months of age, or after the first tooth eruption, as they believe it poses a risk for early childhood cavities (ECC) (American Academy of Pediatrics Dentistry, 2011).
Dental caries is one of the most common chronic diseases in childhood creating severe problems worldwide (Losso et al., 2009). In 2003, the AAPD defined ECC as the presence of one or more decayed (non-cavitated or cavitated), missing (due to caries), or filled tooth surfaces in any primary tooth in a child up to 71 months of age or younger (Iida et al., 2007; Losso et al., 2009; Prakash et al., 2012; Ribeiro & Ribeiro, 2004). The prevalence of ECC is thought to be five times higher than asthma, and seven times higher than allergic rhinitis, ranging from 1% to 12% in preschoolers of developed countries and from 50%-80% in high-risk groups (Prakash et al., 2012; Ribeiro & Ribeiro, 2004). Teeth play an important role in digestion of food, in keeping spacing for the secondary teeth, in helping with speech development and contributing to social skills and confidence (Valaitis et al., 2000). EEC, when left untreated, has been linked with pain, bacteremia,
1 Valerielavigne@me.com
compromised chewing, toxic overdose of analgesics, followed by malocclusion in permanent dentition, phonetic problems, lower self-esteem, and failure to thrive (Azevedo et al., 2005; Prakash et al., 2012). Identifying the risk factors associated with ECC are very important to help prevent the condition, as children often require costly treatment with hospitalization under sedation or general anesthesia (Prakash et al., 2012). The estimation of cost to repair ECC ranges between $200 and $6000 if general anesthesia and hospitalization are required (Udin, 1999).
Causes of Early Childhood Caries
ECC is a disease of multifactorial etiology. The main factors are: a) cariogenic bacteria, b) fermentable carbohydrate diet, c) susceptible tooth and host, d) time (Harris et al., 2004; Losso et al., 2009; Prakash et al., 2012). ECC has also been linked with the following risk factors: demographics characteristics, oral hygiene practice, parental attitudes, educational status of the mother, temperament of child, pacifiers dipped in honey, frequent medication, and feeding habits (Azevedo et al., 2005; Prakash et al., 2012). Another risk factor worth noting from some preliminary studies is the association between the maternal level of vitamin D during pregnancy and the impact on primary dentition and ECC. It showed that mothers of children with ECC had significantly lower levels of vitamin D (Schroth, 2010).
The cariogenic micro-organisms involved in ECC are the Streptococcus Mutans and Streptococcus Sobrinus (Ribeiro & Ribeiro, 2004). The infection of Streptococcus is done by vertical transmission from the mother’s saliva containing high levels of Streptococcus at a very specific time called “window of infectivity.” The severity of ECC has been directly linked to the level of bacteria in the mouth and the early infection. The bacteria have been found to be present as early as six months of age, even before tooth eruption (Losso et al., 2009; Prakash et al., 2012). Caries start with the bacteria infection, which then accumulate and multiply on the teeth biofilm or hard surface. This, combined with the prolonged exposure to carbohydrate, allows for the fermentation of the sugar inside the dental plaque causing enamel demineralization resulting in cavities (Retnakumari & Cyriac, 2012; Ribeiro & Ribeiro, 2004; Udin, 1999).
There is an association between frequency of carbohydrate exposure and caries, and whether the contact occurs mainly between meals and during sleep. During these periods, the saliva decreases and does not flush the carbohydrate away from the teeth, therefore allowing the bacteria to ferment (Losso et al., 2009). Breast milk has been shown to have a higher level of carbohydrate, which could potentially make it more cariogenic (Erickson & Mazhari, 1999). However, the level of cariogenicity of breast milk has been studied and the results showed that breast milk alone, in an in-vitro model, was not cariogenic and did not cause plaque ph reduction and enamel decalcification. Breast milk combined with a sugar rich diet can allow for bacterial fermentation and can become cariogenic (Erickson & Mazhari, 1999). The diet and bacteria level, therefore, play an important role in the development of ECC.
As shown, this disease is multifactorial and controversial amongst different professional associations. This paper will then look at the evidence available in the literature to establish if there is an association between prolonged breastfeeding and ECC.
Method:
To investigate this question, the Cochrane library was searched using the following terms “breastfeeding and dental caries.” A Randomized Control Trial (RCT) was found relevant to the topic (Kramer et al., 2007). PubMed was searched, using the following Mesh terms: “breastfeeding and dental caries.” Limits were added for systematic reviews, which resulted in three relevant articles (Ribeiro & Ribeiro, 2004; Valaitis et al., 2000; White, 2008). Another limit was applied to look for RCT and resulted in the same study already found in Cochrane search. When removing the limits the search produced 212 articles. Some of the relevant and available articles were included in the analysis. PubMed was searched again using other terms relevant to the topic “breastfeeding and dental cavities,” and resulted in 285
articles. Some longitudinal and cohort studies were kept for analysis (Arora et al., 2011; Azevedo et al., 2005; Iida et al., 2007; Mohebbi et al., 2008; Prakash et al., 2012; Retnakumari & Cyriac, 2012; Tanaka & Miyake, 2012). Hand searching through the references of the articles was performed to locate other relevant information (Harris et al., 2004; Losso et al., 2009; Weerheijm et al., 1998).
Results:
The search for the highest level of evidence on dental caries and prolonged breastfeeding revealed only one RCT (Kramer et al., 2007). The cluster RCT looked at the effect of an intervention to promote breastfeeding (Promotion of Breastfeeding Intervention Trial- PROBIT) in Belarus. Children were then followed up at 6.5 years of age to determine the effects on breastfeeding and dental caries. The study randomized maternity hospital units (clusters) and one affiliated polyclinic per hospital with double randomization based on both a random numbers table and a coin flip. The experiment implemented the Baby-Friendly Hospital Initiative in the clusters hospital whereas the control hospital continued their normal practices and policies that were in effect.
The results are based on 17,046 healthy breastfed children from 31 maternity wards. The study results showed an increased rate of any breastfeeding at 3, 6, 9 and12 months. The prevalence of exclusive breastfeeding was seven times higher in the PROBIT group versus the control. At 6.5 years of age, 81.5% of children had a dental examination follow up. The dental examination data were recorded in the PROBIT data form. The results showed no significant difference in decayed, missing, or filled teeth (DMFT) between the experimental and control group. The total number of DMFT in the experimental group was 4.3 (3.7%) and in the control group was 4.2 (3.4%).
The authors then concluded that there is no reduction in caries risk with prolonged and exclusive breastfeeding. The authors addressed a limitation of their study being that routine examinations were performed by a large number of uncalibrated public health dentists. One weakness of the study is that by the age of dental evaluation being 6.5 years, some children may have lost a majority of their deciduous incisors teeth, which may have underestimated the effects. Another weakness to consider is that the study showed an increase in breastfeeding rate with the PROBIT, but the breastfeeding duration is not known for the children that developed caries. Nonetheless, this is a very interesting study due to the large sample size and the randomized experimental design.
Evidence from Systematic Reviews
The next level of evidence to consider was systematic reviews. White (2008) produced a systematic review to answer a clinical scenario using a PICO (population- intervention-comparison-outcome) style question: “does continuation of breastfeeding increase the risk of early childhood caries in infants of over six months of age compared with other methods of infant feeding?” This was a well-performed review. The author described her search strategy and mesh terms used, showed a table of summary of the relevant papers. Her review concluded that there is a lack of consistent evidence linking breastfeeding to the development of ECC. She suggests that an emphasis should be placed on promoting good oral hygiene practice from the time of eruption of the first tooth, and giving parents advice on reducing the frequency and consumption of sugar containing foods and drinks.
Another review by Ribeiro and Ribeiro (2004) looked at ECC and breastfeeding. The study described the ECC problem well, possible etiologies, and the role of breast milk. However, the review did not describe in detail the search strategy used to find the studies. The studies used were displayed in a table, but there were no details on the quality assessment process for the articles in the review. The studies were difficult to compare due to inconsistent results. However, they still were able to conclude that there were no scientific association between human milk and ECC. They do state that this is a complex relation to establish and that there are many variables that can affect the relationship.
Valaitis et al. (2000) produced another systematic review. This review followed a strong methodology, which is described step by step in a table. They offered a description of the ECC problem and showed a figure on the interrelationships of factors in the development of ECC. The review included 28 relevant articles, and the authors did assess the quality of the study. They mentioned that no articles of strong quality were included and only findings from articles rated as moderate and weak were presented. They noted that some of the results of the studies often contradict one another and findings are not always reproducible. However, they still concluded that the evidence does not suggest a consistent and strong association between breastfeeding and ECC. They do suggest that future
research should be performed with more rigorous researchmethods.
Evidence from Cross-Sectional Studies
Some other studies of interest used retrospective cross- sectional data. Nunes et al. (2012) did a retrospective cohort study involving a sample size of 206 low-income children. This study had a clear description of the inclusion and exclusion criteria. They also used a seven- level hierarchical theoretical framework model to control for the variables associated with ECC. The results showed that prolonged breastfeeding was not a risk factor for ECC after adjusting for some confounders. Interestingly, they did state that age, high sucrose consumption between meals, and the quality of oral hygiene were associated with ECC.
Mohebbi (2008) performed a cross-sectional study with a sample size of 504 children. He concluded that milk- bottle-feeding at night should be limited and was associated to ECC, whereas prolonged breastfeeding appears to have no such negative dental consequences. Another study (Iida et al. 2007) looked at a sample size of 1,576 children, aged two-to-five years old. The results of the different models used to analyze the data showed no evidence that either breastfeeding or its duration was independently associated with an increased risk of ECC. One weakness to note from a retrospective study is the data may be subject to recall bias. Also, in this study some of the confounding variables were not adjusted for due to lack of available data. However, this study is definitely worth noting considering the large sample size.
Azevedo (2005), in contrast, showed a positive association between prolonged breastfeeding and ECC. One important element that was not taken at all into consideration, or adjusted for in this study, was the food habits, snacks between meals, which would have an impact on the results. Tanaka and Miyake (2012) showed that breastfeeding for 18 months or longer was positively associated with the prevalence of dental caries, whereas breastfeeding for 6 to 17 months was non-significantly inversely associated with the prevalence of dental caries. Their sample size was 2,056 children, aged 3 years old. The information was obtained by questionnaire, and the study did adjust for confounders. However, a major weakness is that the breastfeeding duration was the period during which the infants received breast milk, regardless of exclusivity. This poses a problem and may have contributed to dental caries if children were exposed to bottles and formula at any point. They do state that the study still may have many confounding factors that cannot be controlled, and therefore no cause and effect relationship should be drawn.
Discussion
After completing this research, the most striking finding is that ECC is a disease of multiple causes. It becomes difficult to isolate one element and a cause and effect when performing studies. When looking at ECC and breastfeeding alone, a link between the two has been difficult to establish. Some factors to consider that may have an effect are the level of bacteria present in the mouth, a susceptible host and a high sugar (sucrose) intake. Breast milk contains carbohydrates and sugar. However, it was only when mixed with other food that this became an issue. Breastfeeding children with higher levels of bacteria may have more ECC when compared to other breastfeeding children with lower levels of bacteria.
Some authors reported that S.mutans may not be able to use lactose, the sugar found in breast milk, as readily as sucrose, found in food or artificial milk, and some breast-milk antibodies may help impede bacterial growth (Mandel, 1996; Rugg-Gunn et al., 1985). One must remember that the bacteria were shown to be transferred from the mother at a specific time in the toddler’s life.
It is also important to understand that the mechanics of breastfeeding versus bottle feeding are very different. When babies breastfeed, the nipple is drawn far back in the mouth and the milk is released into the throat more directly, whereas in bottle feeding the milk pools around the teeth. The use of a bottle is associated with reduced salivary flow, which would cause the fermentable carbohydrate to pool around the teeth and promote the development of ECC (Ribeiro & Ribeiro, 2004).
In my opinion, the most important factor, which is common to many of these studies, that contributes to ECC is the level of sugar rich food and between meal snacks that are consumed. This, combined with a high level of bacteria, seems to contribute to ECC. It is then crucial that parents be informed on proper dental hygiene for their children from infancy, and be sensitized towards the appropriate non-cariogenic snacks to feed them. Therefore, the mother’s decision to continue breastfeeding should not be affected by the appearance of dental caries in their children, as no solid research has shown a direct link between the two.
Conclusion
Mothers should be encouraged to breastfeed as long as they desire since no conclusive evidence has established
a relationship between prolonged breastfeeding and the development of ECC.
Dr. Valerie Lavigne
Chiropraticienne, DC
A Narrative Review and Case Report:Frenotomy Procedure in Neonate with Tongue-Tie
Lavigne V. A Narrative Review and Case Report: Frenotomy Procedure in Neonate with Tongue-Tie, J Clin Chiropr Pediat. 2012;13:1025-1031.
view the whole article here (pdf)
Introduction:
Mothers around the globe are encouraged to breast- feed according to the recommendations of the World Health Organization that stipulate that infants should be exclusively breastfed for at least the first 6 months of their lives.1 However, for some mothers this guideline may be difficult to follow when they experience challenges. Mothers with breastfeeding difficulties often present to a chiropractor for an assessment of biomechanical dys- function interfering with breastfeeding.2 During the as- sessment of the breastfeeding case, the mouth and tongue motion should be evaluated to determine the presence of tongue-tie.3 The International Affiliation of Tongue- Tie Professionals defines tongue-tie as “an embryological remnant of tissue in the midline between the undersurface of the tongue and the floor of the mouth that restricts normal tongue movement.”4 The tongue-tie’s effect on breastfeeding has been associated with sore nipples, poor infant weight gain, neonatal dehydration and shorter breastfeeding duration.5-7 Considering the controversy amongst professionals regarding the frenotomy procedure, a treatment option for tongue-tie (anky- loglossia), this case report and review of the literature will help determine the necessity of the procedure.
Clinical Presentation
A 28-year-old primiparous mother with breastfeeding difficulties presented to the chiropractic clinic. The mother had a vaginal birth at 39 weeks with an epidural injection for pain control. Birth weight of the neonate was 7 pounds 1 ounce. From the first feed, the mother experienced pain and discomfort. The hospital nurse assisted to improve the latch without success. At initial latch-on, the pain was rated by the mother as a 7/10 and went down to 4/10 during the feed. The discharge weight of the baby was 6 pounds 3 ounces, which was approximately equal to a loss of 9% of the neonate’s birth weight.
Once home, there was minimal improvement of the latch. Both nipples had started bleeding and cracking. The initial latch-on pain was rated at 7/10 but it reduced to 3/10 as the feed progressed. The mother was nursing 8-10 times per day with no supplementation. The neonate was void- ing 6-8 times per day and had 4 stools of yellow color and mustardy texture. The mother contacted her chiropractor who was also an International Board Certified Lactation Consultant (IBCLC) for evaluation and lactation support.
Upon examination, the three-week-old neonate seemed alert and well. The current weight was 7 pounds 3 ounces. He had regained his birth weight and had been gaining on average 0.5 ounces per day since birth. Weight gain should be 15-30 gm/day or 0.5ounces-1.05 ounces per/day. According to the WHO, a fully breastfed girl gains an average of 1,000 grams in the first month, 900 grams in the second month, 700 grams in the third month, and 600 grams in the fourth month of life. A fully breast-fed boy gains an average of 1,200 grams in the first month of life, 1,100 grams in the second month, 800 grams in the third month, and 600 grams in the fourth month.10
The musculoskeletal assessment revealed restrictions in the mandibular excursion, hypertonicity in the scalenes, sternocleidomastoid, temporalis and masseter muscles. Evaluation of the cranial and vertebral motion using mo- tion palpation and craniosacral technique showed cervical dysfunction at C1 and dysfunction of the parietal, frontal and temporal bones. The mouth and tongue examination revealed the presence of a short, thin lingual frenulum that was attached to the lower ridge of the gum line. Tongue motion was restricted in three planes, elevation and lateral motion were reduced and extension could not reach past the lower gum line. When lifting the tongue, the heart shape associated with a tight anterior frenulum was visible.
The chiropractor, IBCLC assessed the sucking and could feel the lower gum hitting her finger with reduced cupping of the tongue. To evaluate the tongue-tie, the doctor used the Hazelbaker Assessment Tool for Lingual Frenulum Function (HATLFF) and the Frenotomy Deci- sion Rule for Breastfeeding Infant (FDRBI). The HATLFF function score was 6/14 and the appearance score was 3/10. Many components of the FDRBI tool were positive for the mother-baby dyad. An examination of the mother’s nipples revealed bilateral cracks at the base. Following visual exami- nation, the baby was put to breast to assess feeding. Even after latch adjustments, craniosacral treatment and soft tis- sue therapy, the pain did not decrease. The baby continued to receive craniosacral therapy and chiropractic treatment to the problematic area, but the mother was informed as well that a frenotomy procedure could potentially decrease the pain.11,12 To help the mother understand the procedure and make a decision, the question to be answered was does a frenotomy alleviate breastfeeding difficulties in a neonate with tongue-tie?
Literature Review
Method
The starting point for an evidence-based search was the Cochrane Library. The decision was made to start with the terms of the question. The database search was executed with “tongue-tie” and resulted in two randomized
control trials.13,14 Searching the database using “ankyloglos- sia” produced one methodological review,9 six trials and one technology assessment from the National Institute for Health and Clinical Excellence.15 Three of the trials were abstracts only and one was not retained because it used different treatments.5,16 Searching with “frenotomy” revealed nothing new.
Another database search using PubMed was done by combining the previous terms with “breastfeeding” using the Boolean operator “and”. A first search with “anky- loglossia and breastfeeding” produced 42 papers. Limits of “randomized control trials (RCT), practice guidelines and review” were added which resulted in 9 papers. Most had already been found.17 A second search with the same limits was performed with “tongue-tie and breastfeeding” and resulted in 15 papers. A third search using the MeSH terms “lingual frenum/abnormalities and lingual frenum/ surgery” produced 107 articles. The same limits as earlier resulted in 17 papers most of which were previously found. To assess the risk of complications of the procedure, the PubMed search was performed using the terms “frenotomy and complications”. No new articles were retrieved except for a new case series.18
Results:
The search revealed that only a small number of studies such as randomized controlled trials (RCT) and systematic reviews were available. However, even with a small number of studies, the National Institute for Clinical Excellence established the first guidelines in December 2005 and reviewed them in February 2011 without much change. The specialists that wrote these guidelines came from vari- ous health fields. The inclusion criteria for studies were well defined. When the guidelines were written only one RCT14 was available and a few case series.19-21 The revised guidelines state that “current evidence suggests that there are no major safety concerns about division of ankyloglossia (tongue-tie) and limited evidence suggests that this proce- dure can improve breastfeeding. This evidence is adequate to support the use of the procedure provided that normal arrangements are in place for consent, audit and clinical governance.”22 The guidelines mention that frenotomy should be performed by registered healthcare professionals who are properly trained and that there is a need for further controlled trials on the long-term effect on breastfeeding. They also state “there were conflicting opinions among the Specialist Advisors and some stated that it is difficult to be certain whether any perceived improvement in breast- feeding is due to division of the tongue-tie.” One would assume that this conflict was not strong enough to affect the guidelines recommendations.
Berry et al. (2012) produced a double-blind random- ized controlled trial on tongue-tie division in Southampton, UK. The aim of this study was to see if maternally reported improvement in breastfeeding after the tongue tie division was due to the placebo effect. They had 66 babies from 5-115 days old. They were randomized to a division group and a non-division group. The mother and trained observer were blinded. The results showed an immediate improve- ment in feeding in 78% of mothers in the division group compared to 47% in the non-division group. This study was very well performed however one weakness to note is that they did not grade the tongue-tie. It was therefore difficult to know if these babies had anterior or posterior tongue-tie.
Buryk et al.(2011) produced another randomized single-blinded trial. Newborns with significant ankyloglossia and problems breastfeeding were followed over a 12-month period. Fifty-eight newborns were divided into two groups: 30 infants in the frenotomy group and 28 in the sham group.The diagnostic tool for ankyloglossia used was the HALTFF. Other parameters such as the nipple pain scale and the Infant Breastfeeding Assessment Tool were used. They followed up at 2 weeks and regularly over a one year period. Both groups showed statistically significant decreases of pain scores after the intervention but the frenotomy group improved significantly more than the sham group. Breastfeeding scores improved significantly in the frenotomy group (p=.029). This ap- pears to be a well executed RCT however, with a small sample size. The authors decided to quantify the nipple pain and the breastfeeding capacity of the newborn which adds value to this study. One major issue with tongue-tie remains identifying which tongue-tie require frenotomy. This study used the HALTFF tool since it is the only vali- dated and reliable screening tool that considers function and appearance of the tongue in babies under 6 months.23,24 The HALTFF tool can be used to determine tongue-tied neonate regardless of the feeding method. However, when working in a breastfeeding clinic where the focus is solely on breastfeeding considering the maternal signs and symptoms are very important factors when deciding to do the frenotomy. In the breastfeeding relationship, one needs to look at the dyad i.e. mother and baby. Since the HALTFF tool does not include the mother’s complaint or integrity of her nipple to determine if the frenotomy is needed, it would be helpful in a breastfeeding situation to add another tool when determining the need for the frenotomy. Such a tool (FDBR) has been developed to help identify anterior tongue-tie however it has not been validated.25 This tool was also used in a prospective un- controlled study and it incorporates both the appearance and function of the tongue and the maternal signs and symptoms. Combining these two tools may help emphasize when the frenotomy is necessary for breastfeeding moth- ers if the HALTFF score is borderline but the mother is experiencing much pain.
In the aforementioned study’s discussion, the authors also reviewed the weaknesses, limitations and biases. An important bias was that mothers were motivated to breastfeed. One weakness involved the blinding process. The mothers were asked not to look in their baby’s mouth after the procedure and this is very hard to control. Also, all the patients in the control group were offered the procedure at the two-week mark and all but one mother opted for the frenotomy. This eliminated any possibil- ity for more comparison between the groups. This study did not help the practitioner determine what the best timing was to perform the frenotomy but, overall a well- designed study that showed that breastfeeding mothers whose baby were struggling could be helped by a simple frenotomy.
Dollberg et al.(2006) produced a randomized, pro- spective study that looked at 25 infants with ankyloglossia and mothers with nipple pain. It found “after frenotomy, there was an immediate and significant nipple pain relief as judged by a significant decrease in pain score after frenotomy then after sham”5 The trial was blinded and randomized in two sequences: 1) frenotomy followed by breastfeeding followed by sham followed by breastfeeding and 2) sham followed by breastfeeding followed by freno- tomy followed by breastfeeding. Throughout the entire process, the authors ensured that the mother was blinded to the frenotomy procedure by having an investigator present during breastfeeding following the procedure. This made sure she did not look in the baby’s mouth. The study did not use a validated tool for the identification of the tongue-tie but used a more subjective tool. This would make it difficult for a practitioner in the field to identify which tongue-tie would need frenotomy. Despite its small sample size, the frenotomy procedure had positive results.
The Hogan et al. (2005) study was used in the formula- tion of the National Institute for Health in Clinical Excel- lence (NICE) guidelines. The study included 57 babies with tongue-tie of which 40 were breastfed and 17 were bottle-fed. After 4 weeks of normal monitoring, if feeding problems emerged possibly due to a tongue-tie, they were sent for a thorough assessment. They were randomized into two groups: one that offered intensive support, advice and support from the IBCLC (control) and one that had an immediate frenotomy. There were 28 children (20 breastfed and 8 bottle-fed) in the frenotomy group and 29 children in the control (20 breastfed, 9 bottle-fed). The improvement at 48 hours for the frenotomy group was statistically signifi- cant with 27/28 children improving in the division group versus 1/29 in the control group. In the breastfed baby group, 19/20 babies improved with frenotomy whereas only 1/20 improved without frenotomy, a statistically sig- nificant difference. All the remaining mothers in the control group, all requested tongue-tie division after the 48 hours of intensive lactation support and 27/28 babies improved. The overall improvement with feeding after frenotomy was 54/57 (95% of infants). This study showed that tongue-tie may also have an impact on either breastfeeding or bottle feeding. The randomization process was well explained. They found that there was no association between tongue- tie length and feeding difficulty meaning that by looking only at the tongue-tie, they could not predict which one was causing breastfeeding difficulties as some babies with 100% tongue-tie were breastfeeding asymptomatically. One major weakness involves the identification process of tongue tie where clinical inspection was used. Even with a small number of subjects, it was still able to show statisti- cal significance. It did not use however any quantification method to assess feeding pain. This being one of the first randomized trials, it was a good foundation for future researchers to improve upon.
Steehler et al. (2012) produced a retrospective review of frenotomy in infants with breastfeeding difficulties. This cohort study and retrospective review was done by gathering data and then following up with a telephone survey. The results showed that 367 neonatal and infant consultations were performed for feeding difficulties and 307 infants underwent a frenotomy and 91 mothers participated in the follow up telephone survey. It showed that 80.4% of the mothers believed that the procedure strongly benefited their child’s ability to breastfeed, and 82.9% of the mothers were able to initiate or resume breastfeeding after the procedure. A very interesting result is that they showed more benefits when the procedure was done in the first week of life of the infant. This would be interesting to follow up upon to assess what is the best timing to perform the procedure. One weakness of retrospective study is always the recall bias that cannot be removed however an interesting study that looks at the timing of the procedure.
The Cochrane search resulted in a methodological re- view which was a clear and concise review of the literature on ankyloglossia/tongue-tie9 The aim of the study was clearly defined. The database sources were identified and synthesis of the studies well explained. All the articles werenalyzed by two of the authors independently and reached a consensus on the results. Their results showed that a diagnostic criteria is needed to allow better comparison between studies. It also showed that frenotomy is likely an effective treatment but more trials are necessary and that a reliable frenotomy decision rule is needed.
Another well executed literature review by Suter and Bornstein (2009) came to similar conclusions concerning the lack of uniform definitions and classifications. It also questioned which tongue-tie need intervention.
Regarding the risks and safety of the procedure, all the trials reported very few complications. The NICE guide- lines list as potential risks: bleeding, infection, ulceration, pain, damage to the tongue and salivary glands. However, several advisors state these as very rare events. They have not been reported in any of the trials except for minor bleeding. One very small case series of only two patients though reported severe bleeding.18 The conclusion was that frenotomy should be performed by trained professionals to avoid complications. Considering that over 134 babies in the 3 previous trials showed no major complications, one could infer that if performed well, the frenotomy is a safe in- tervention. The parents should ensure that the professionals are well trained in the procedure before giving their consent to perform the procedure on their neonate/infant.
Interpretation of the Evidence:
The evidence found on frenotomy and breastfeeding was discussed with the patient. The decision was made as follows:
- This patient had tried conservative care with an IBCLC with little improvement
- This patient was presently under care to resolve the musculoskeletal components
- Her HATLFF score indicated a need for frenotomy
- Many aspects of the FDRBI tool were present
- The NICE guidelines recommended frenotomy based on the available evidence
- Since these guidelines had come out in 2005, other RCTs had been produced with positive results
- Most of the studies except for a small case series were showing no serious complications associated with the frenotomy
- The NICE guidelines and all the studies recom- mended that the procedure be performed by trained professionals
Intervention and Outcomes
This mother was referred to a breastfeeding clinic where trained professionals perform the frenotomy procedure daily. The mother received her informed consent and agreed to the procedure. The baby experienced minimal bleeding and remained calm during the procedure. After the freno- tomy, the baby went to the breast with a dramatic reduction in maternal pain. Over the next few weeks, the mother’s pain continued to decrease and her nipple damage healed. Follow up care for the frenotomy procedure was provided by the breastfeeding clinic and the author continued to follow this neonate for the musculoskeletal problems.
Conclusion
This case showed that frenotomy, if performed by trained professionals, can improve breastfeeding and should be considered to help the mother-baby dyad. This case report demonstrates how the chiropractor can easily apply the appropriate assessment tools along with therapeutic techniques to assess, treat and recommend the appropri- ate consultations and or interventions for women who are experiencing breastfeeding difficulties secondary to tongue tie in their children.
Dr. Valerie Lavigne
Chiropraticienne, DC